[ad_1]
RESEARCH – SURVEY
Childhood vaccine status and correlation with common nonvaccine-preventable illnesses Michelle M. Anderson, DNP, FNP (Family Nurse Practitioner)1 & Cathy Arvidson, PhD, FNP, RN, FAANP (Associate Professor)2
1Pend Oreille Health Care, Sandpoint, Idaho 2School of Nursing, Idaho State University at Pocatello, Idaho
Keywords Children; immunization; illness; pediatric;
vaccination; nurse practitioner; advanced
practice nurse; preventive health services.
Correspondence Michelle M. Anderson, 1207 Michigan Street,
Suite C, Sandpoint, ID 83864. Tel: 208-265-2221,
Fax: 208-265-2229; E-mail:andemic9@isu.edu
Received: 28 October 2016;
revised: 10 March 2017;
accepted: 10 March 2017
doi: 10.1002/2327-6924.12464
Abstract
Background and purpose: Current trends in parental decision making involve alteration from vaccine schedules in children, citing concerns for altered immune function. The purpose of this study was to determine if there is a difference in incidence of common childhood illnesses dependent on vaccination status. Methods: An investigator-designed survey was administered to parents of chil- dren aged 12 months to 7 years. Participants were separated into one of three groups: fully vaccinated, partially vaccinated, and unvaccinated. There were 111 total participants. Power analysis indicated a minimum of 30 participants per group to detect an 80% effect. Descriptive statistics were applied to variables with chi-square for group comparison. Conclusions: The results indicated a statistically significant difference between all three groups in the categories of ear infections, influenza, and common colds. Fully immunized group had significantly more ear infections than partial or unimmunized. The unimmunized group had significantly more colds and flu. Implications for practice: Nurse practitioner practice implications relate di- rectly to further education of parents, support, and trust building. Many parents question the possible association between childhood vaccines and immune func- tion and have a distrust of current research. This study showed that most com- mon childhood illnesses are equitable across the population and not dependent on vaccine status.
Introduction
Vaccines have long been considered one of the great- est public health accomplishments of the last century (In- stitute of Medicine [IOM], 2002). With the introduction of vaccines, smallpox has been eradicated globally and the rates of other communicable diseases, such as polio and measles, have drastically reduced (Andre et al., 2008; Epling, Savoy, Temte, Schoof, & Campos-Outcalt, 2014). During the last 20 years, the Centers for Disease Control and Prevention (CDC) have updated the childhood immu- nization schedule to include newer vaccines such as PCV- 13 and meningococcal. As a result, children receive multi- ple vaccinations during each well-child visit, especially in their first year of life leading to a balance of ensuring nec- essary vaccines and minimizing parental and child discom- fort and stress (Bakhache et al., 2013). The Healthy People 2020 goal is for a vaccination rate of 80% or higher for all
children in the United States (Office of Disease Prevention and Health Promotion [ODPHP], 2015).
A current trend however is numerous parental refusals of vaccinations for their children or requests for par- tial administration (Connors et al., 2012; Gust, Darling, Kennedy, & Schwartz, 2008; Yaqub, Castle-Clarke, Sev- dalis, & Chataway, 2014). One of the prevalent parental reasons for this decision relates to their perceived uncer- tainty about both short-term and long-term immune sys- tem effects with the large volume of vaccines administered (Bakhache et al., 2013; Byström, Lindstrand, Likhite, But- ler, & Emmelin, 2014). This perceived uncertainty has led to an ever increasing group of people making alternative choices to the immunization schedule and in some cases choosing to not vaccinate their children at all. With this trend we have seen the reoccurrence of what were previ- ously considered eradicated diseases, such as measles. Pre- vious studies have looked at barriers to vaccination and
415Journal of the American Association of Nurse Practitioners 29 (2017) 415–423 C©2017 American Association of Nurse Practitioners
Childhood vaccine status M. M. Anderson & C. Arvidson
Byström et al. (2014) found that parents highlighted the need for vaccine information from sources unbiased from pharmalogical company influence. Some parents have un- substantiated concerns about the effect of multiple immu- nizations on their children’s immune system. These par- ents have concerns that it could make their children more susceptible to childhood illnesses. There is little research about the effect of immunizations on other childhood ill- nesses. The purpose of this study is to determine if there is a difference in incidence of common childhood illnesses dependent on vaccination status.
Background
The ODPHP (2015) has a stated Healthy People 2020 goal of an 80% vaccination rate for children in the United States. The World Health Organization (WHO; 2009) has a goal of 90% national vaccination coverage and at least 80% in every district (type of administrative division) or equivalent in all countries. The current vaccine data in the United States for the age range of 19–35 months show the national average at 70.4% in 2013 (ODPHP). Although this number has increased from the baseline in 2009 of 44.3% it is still not at the Healthy People 2020 goal. Instead, the rate of partial or nonvaccination is in- creasing. The literature between 2004 and 2011 shows the partial or nonvaccinating rate to be anywhere between 1.48% and 2.2% up to 26% depending on the state and demographic area, with the Pacific region of the United States having a higher rate of nonmedical vaccine ex- emption (Siddiqui, Salmon, & Omer, 2013). Glanz et al. (2013) conducted a retrospective matched cohort study looking at children between the ages of 2 and 24 months from 2004 to 2008, and found that 48.7% were under- vaccinated before the age of 24 months. Many studies allude to the reasons for vaccine hesitancy, listing trust in the products and the system behind them, reactions to the product, and fear of altered childhood immune function.
Several researchers show that an increasing trend in vac- cine delay or hesitancy is because of immunization suc- cess. The advantages, efficaciousness, and safety of vac- cines have been widely supported scientifically (Schmitz, Poethko-Müller, Reiter, Schlaud, & Twisselmann, 2011). Epidemiology data demonstrate that vaccine-preventable diseases have been reduced and in some cases in the United States, completely eliminated. The challenge is that the parents of young children, as well as their younger healthcare providers, are no longer familiar with vaccine- preventable diseases shifting fear from the disease to po- tential vaccine reactions (Epling et al., 2014; Fernbach, 2011; Salmon, Dudley, Glanz, & Omer, 2015). In a study by Martin and Badalyan (2012), 21% of specialty pedia-
tricians and 9% of general pediatricians are found to de- viate from the recommended Centers for Disease Control and Prevention (CDC) guidelines when considering vacci- nation for their future child citing safety concerns as their rationale.
Trust in vaccine information and how the informa- tion is presented is at an all-time low which is con- tributing to parental vaccine delay or refusal (Offit & Moser, 2009; Siddiqui, Salmon, & Omer, 2013). Yaqub et al. (2014) completed the first consolidated overview of parental vaccine attitudes and found that when parents distrust the medical information, they will re-interpret the medical report. Personal and strongly held beliefs will play a role in this re-interpretation. Additionally, Yaqub et al. found that parents distrusted official sources of vac- cine information because of commercial interests, such as monetary gain, or the sense of being an overzealous vaccinator.
With an ever-changing immunization schedule and the addition of new vaccines, the total vaccines administered in a child’s first 18 months of life, when everything is ad- ministered on time, are 25 inoculations (ODPHP, 2015). Fernbach (2011) found that parents have a growing con- cern that an infant’s immune system is too immature to respond correctly to such a large vaccine load. Fern- bach went on to describe that this conclusion is not sup- ported by research and that passive immunity acquired from the mother, through the development of B and T cells in utero combined with the innate neonatal immune re- sponse, does not result in an increased infection rate after immunization.
Bakhache et al. (2013) and Salmon et al. (2015) found that 25%–38% of parents have a concern regarding their child’s immune system being overworked. Parents feel when an immune system is regarded as overworked, sus- ceptibility and subsequent incidence for common illness is believed to rise. Common childhood illnesses can be bacte- rial and/or viral. They can include: fever, cough, diarrhea, vomiting, and skin rashes (Angoulvant et al., 2013; Bryant & Lester, 2014). Common childhood upper respiratory tract infections include otitis media, otitis externa, sinusi- tis, and pharyngitis (Alter, Vidwan, Sobande, Omoloja, & Bennett, 2011). Also commonly seen is conjunctivi- tis. Less common, but still highly prevalent, is bacterial pneumonia, urinary tract infections, and gastroenteritis. Pneumonia is the most common cause of death in a child under the age of 5 worldwide (Scott & English, 2008).
Literature review
More recent studies are starting to look at vaccine hes- itancy and address some of the associated questions and reasons. Schmitz et al. (2011) utilized data collected over
416
M. M. Anderson & C. Arvidson Childhood vaccine status
a 3-year time frame from the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) to evaluate whether there are differences in lev- els of health between unvaccinated children and adoles- cents. The theory is that vaccines overburden the immune system leading to increased illness among the vaccinated group. The researchers focused on allergic diseases such as atopy as well as common childhood infections such as colds and flu. Children from the ages of 1 to 5 were found to have the highest numbers of infections. This age range also showed a lower median number of infectious diseases in the unvaccinated group (3.3) when compared to the vaccinated group (4.2) but this was not statistically significant.
Siddiqui et al. (2013) reviewed the epidemiology of vac- cine hesitancy in the United States. They found several reasons listed for this hesitancy which included: lower per- ceived vaccine safety and efficacy, lower perceived disease susceptibility and severity, and lower trust in the vaccine source of information. Harm and an overworked immune system were the most cited safety reasons given by parents. For this reason many parents opt for an alternative sched- ule for vaccination. They concluded that ongoing surveil- lance of vaccine hesitancy will provide valuable informa- tion on specific tools healthcare providers can best utilize for educational purposes.
Byström et al. (2014) explored decision-making atti- tudes of 20 parents from an anthroposophic community, differentiating between those who chose to vaccinate and those who did not. Even though this was a small sample size (n = 20), they cited uncertainty about long- and short- term vaccine effects on a child’s health, immune function overload, and doubts about safety as the compelling rea- sons for each parent’s choice. Nonvaccinating parents tend to carry a holistic or alternative view on health, utilizing other components to health aside from risk of illness, and prefer to wait for their child’s immune system to fully de- velop before challenging it. These choices came from con- cern on vaccine safety. Both parental groups talked about the need for information on vaccines to be available from unbiased sources.
Kiraly et al. (2016) found that when immunizations are given before 12 months of age that children can have a potentially altered immune system. The study found that children with delayed DTaP had reduced odds of trigger- ing eczema compared to those vaccinated on time. One theorized reason is that the aluminum adjunct common in DTaP vaccines can be a T helper (TH) 2 stimulant which has been known to cause TH2 polarization which is associated with food allergy and atopic eczema. The study concluded that there was no association between delayed DTaP vac- cine and food allergy, but there was less eczema and use of eczema medication. The researchers felt that the timing of
routine infant vaccines may affect susceptibility to allergic disease.
What seem to be missing in the current literature are studies assessing the association between vaccines and typ- ical childhood illnesses, such as the common cold, flu and ear infections. Ear infections can be of bacterial or viral etiology, with strep pneumoniae being a prevalent bacte- rial cause. Additionally, several studies note that parents have a growing concern over the risk of the amount of vac- cines given at a single visit as well as the increased number of vaccines given in the first 3 years of life. Many studies look at different components of this area but the lack of a study involving a comparison between a fully vaccinated (FV), partially vaccinated (PV), and nonvaccinated (NV) group is missing. These three groups exist and are present in the United States; however, there is no information di- recting healthcare providers on how to answer the ques- tions they are being asked when parents are starting to question vaccines and become vaccine hesitant.
Hypothesis
The hypothesis for this study is that there are no differ- ences between FV, PV, and NV groups in the frequency of common vaccine-preventable childhood illnesses.
Methods
The study was approved by the Idaho State University Institutional Review Board.
Setting
The study was conducted at a nurse practitioner-owned (NPO) family practice in North Idaho. The state of Idaho offers free vaccines to children until the age of 19, in- clusive of all insurance levels or uninsured status, there- fore insurance coverage and the ability to pay for vac- cines did not play a role in inclusion to this study. In this NPO office, the majority of vaccinations are administered to children under the age of 7 usually within the first 12 months of life per standard of care guidelines (ODPHP, 2015). The illnesses listed on the survey were those com- monly seen and evaluated in primary care practice as well as cited in other similar studies of children of this age group (Angoulvant et al., 2013, Schmitz et al., 2011).
For the purpose of this study, FV status is defined as all required immunization for school entry, which includes: age appropriate dosing of DTaP; poliovirus vaccine; Hib vaccine; measles, mumps, and rubella vaccine; and vari- cella vaccine (Dunn et al., 2015). Hepatitis A and B, PCV- 13, and rotavirus vaccines will be counted but not required for status as full vaccination as they are not required for
417
Childhood vaccine status M. M. Anderson & C. Arvidson
school entry. These are the vaccines scheduled during the first year of life with additional doses during the child’s first 6 years. PV status will include one or more vaccines, but not include all of them. NV status is defined as no vaccines at the time of administration of the questionnaire.
Instrument
The survey was designed with a mix of closed-ended and open-ended questions. There was a list of common child- hood illnesses listed based on the literature review, num- ber of times, and age of illness if remembered. The open- ended questions involved filling in age of child, number of other children in the household, their ages, and the par- ents’ choice for what had guided their vaccine decision. The survey was validated with a comparative chart review of the listed illnesses in the participant’s medical record. The parental recall response correlated with the medical record review with an accuracy of 85%.
Sample
A nonprobability sample (convenience sample) was used. The study reviewed three separate groups of children aged 12 months until 7 years: FV group, PV group, and NV group. The survey was offered to parents once during the enrollment period of August through December 2015. During this same period, the researcher completed a chart review on each child using an identical survey. Inclusion criteria included: children between the ages of 12 months and 7 years presenting to the NPO for a visit during the re- ported study time. Exclusion criteria included any children outside of the study age range and or a history of chronic illness, immunocompromised status, or known congenital defects. A power analysis for a Wilcoxon signed-rank test determined a minimum of 30 participants per group for an 80% effect.
Procedure
All parents of children meeting the inclusion criteria seen in the practice during the enrollment period were asked to participate in the study. A consent form was given to each parent by the medical assistant when they were taken to the exam room. If they agreed to be in the study, the parents were asked to complete the question- naire while in the exam room. The survey was anonymous and there was no identifying data.
The parental survey included the child’s age, vaccine sta- tus, reason for vaccine choice, vaccines already given, day- care or school status, number and ages of other children in the household, number of office visits (to be completed by the provider with a chart review), and a list of common
childhood illnesses with instructions to list yes/no for each occurrence, a column for number of times per lifetime, and a separate column for age of illness occurrence. The survey took 10–15 min to complete. Each completed question- naire was assigned a number which corresponded with the subjects’ name on a separate list which was kept separately in a locked cabinet in the researcher’s office. Following ad- ministration of the survey, the researcher completed a ret- rospective chart review confirming previous vaccine ad- ministration and added the number of documented office visits. Whenever possible and/or relevant, previous med- ical records from another health facility were reviewed for completeness of vaccination history and number of of- fice visits. The Idaho Immunization Reminder Information System (IRIS), a state vaccine registry, was checked to con- firm vaccine status.
The response rate of the survey was 97.6%; 81 parents of 83 approached agreed to participate. This was higher than expected and was likely because of the enthusiasm and neutrality of presentation of the study. The complete- ness of the responses was as expected for a parental recall survey.
Data analysis
The data were entered into an Excel Spreadsheet to uti- lize count data and one section for description for reason of vaccine choice. The qualitative data from the open-ended questions were evaluated and grouped into like categories.
Descriptive statistics were calculated for all variables. Parental survey responses to nominal variables (illness/no illness, yes/no, school attendance) were compared across three groups of children (FV, PV, and NV). Chi-square tests were completed to test the categorical survey data and to determine whether a significant association between groups exists. Specifically, testing for an association be- tween groups and at least one illness episode was studied. A one-way ANOVA was used to determine if there were any significant differences between the means of the three groups related to age and number of office visits.
Results
Demographic characteristics
Eighty-one parents answered the survey for a total of 111 participant children. The mean age of all children was calculated at 3.5 (SD 2.0) with a median of 3.0. The mean age of the FV group was 4.0 (SD 1.9), PV group was 2.97 (SD 2.0), and NV group was 3.51 (SD 2.0). There was no statistical difference in mean or median age between the groups.
418
M. M. Anderson & C. Arvidson Childhood vaccine status
Figure 1 Distribution of children among the groups (n = 111).
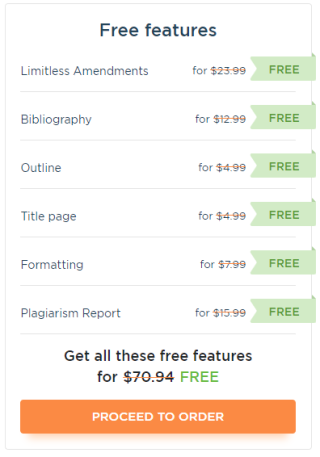
There was an equitable distribution between the three groups in the study with 31% in the FV group (n = 34), 32% in the PV group (n = 36), and 37% in the NV group (n = 41; see Figure 1). The most commonly given vaccine in both groups was the DTaP with 100% coverage in the FV (n = 34) and 85.1% (n = 31) in the PV group. Table 1 lists the distribution of coverage among these two groups.
Findings
A chi-square test for group association to determine sta- tistical significance for the most commonly occurring ill- nesses was completed. There were enough listed illnesses in seven of the surveyed common illnesses to allow for this testing (Figure 2). The other areas, although interesting and with some promise to show a difference, like eczema, were not large enough for comparison (Table 2).
Table 1 Distribution of vaccine coverage between groups
Vaccine Fully immunized n = 34 (%) Partially immunized n = 36 (%)
DTaP 34 (100) 31 (85.1)
Varicella 29 (85.3) 6 (16.7)
HepA 29 (85.3) 4 (11.1)
Hib 34 (100) 21 (58.3)
PCV-13 34 (100) 12 (33.3)
IPV 32 (94.1) 15 (41.7)
MMR 32 (94.1) 12 (31.3)
HepB 31 (91.2) 4 (11.1)
Note. n = 70
The FV group showed a statistical difference (p < .0005) in the comparison of ear infections when compared to the PV group and the NV group. Out of the total number of reported ear infections (n = 51), the FV listed a 50.9%
Figure 2 Bar graph of group experienced illness (n = 111).
419
Childhood vaccine status M. M. Anderson & C. Arvidson
Table 2 Illnesses experienced among the three groups
Children with
illness
Fully vaccinated n = 34 (30.6%)
Partially
vaccinated n = 36 (32.4%)
Not vaccinated n = 41 (36.9%)
Total number with
Illness p-Value
Ear infection 26 (50.9) 10 (19.6) 15 (29.4) 51 <.0005
Cough 27 (32.5) 26 (31.3) 30 (36.1) 83 .753
Fever 30 (31.6) 29 (30.5) 36 (37.9) 95 .578
Flu 14 (30.4) 10 (21.7) 22 (47.8) 46 .056
Diarrhea 19 (32.2) 18 (30.5) 22 (37.3) 59 .883
Vomiting 24 (36.3) 17 (25.8) 25 (37.9) 66 .126
Cold 30 (30.6) 28 (28.6) 40 (40.8) 98 .023
Pneumonia 0 1 (2.8) 0 1
Croup 1 (2.9) 2 (5.6) 5 (12.2) 8
Sinusitis 3 (8.8) 1 (2.8) 0 4
Conjunctivitis 6 (17.6) 3 (8.3) 6 (14.6) 15
Hand/foot/mouth 7 (20.6) 2 (5.6) 1 (2.4) 10
Pharyngitis 6 (17.6) 1 (2.8) 0 7
Tonsillitis 1 (2.9) 0 0 1
Chickenpox 0 1 (2.8) 0 1
Measles 0 0 0 0
Whooping cough 0 0 1 (2.4) 1
Bronchiolitis 1 (2.9) 0 0 1
Eczema 5 (14.7) 2 (5.6) 3 (7.3) 10
Other 2 1 0 3
Table 3 Reasons given for vaccination choice
Reason Fully vaccinated n = 34 (%) Partially vaccinated n = 36 (%) Not vaccinated n = 41 (%)
Adherence to guidelines 4 (16.6) 0 0
Advice—healthcare
providers
3 (12.5) 1 (4.3) 1 (2.9)
Advice—other people 0 0 2 (5.7)
Alternative schedule 2 (8.3) 8 (34.8) 0
Concerns—ingredients 0 0 5 (14.3)
Concerns—reactions/side
effects/immune system
response
2 (8.3) 7 (30.4) 2 (5.7)
Health reasons 2 (8.3) 0 4 (9.8)
Philosophical/personal beliefs 1 (4.2) 2 (8.7) 3 (8.6)
Research 6 (25) 5 (21.7) 17 (48.6)
Travel plans 3 (12.5) 0 0
Other 1 (4.2) 0 1 (2.9)
Total with responses 24 (70.5) 23 (63.9) 35 (86.4)
Missing responses 10 13 6
Total 34 36 41
occurrence rate (n = 26) compared to 19.6% (n = 10) and 29.4% (n = 15), respectively.
A second statistical association was observed between the three groups and influenza (flu; p = .056). Influenza occurred 46 times between the three groups. The NV group had a 47.8% occurrence (n = 22) when compared to FV (30.4%; n = 14) and PV (21.7%; n = 10).
The common cold (n = 98) was the final significant ob- servation. The NV group had a statistically relevant finding
(p = .023) with a 40.8% occurrence of colds (n = 40) in comparison to FV (30.6%; n = 30) and PV (28.6%; n = 28). No other statistical association was noted between the three groups and the occurrence of any illness.
Baseline comparisons of number of office visits between the three groups were determined using the mean. Mean number of visits for the FV group is 6 (SD 5). Mean number of office visits for the PV group is 7 (SD 4). Mean number of office visits for the NV group is 6 (SD 4). Overall, 49% of
420
M. M. Anderson & C. Arvidson Childhood vaccine status
children had 5 or fewer office visits (range 2–5) and 51% had more than 5 (range 6–22).
Parental attitudes concerning vaccination were ex- amined. Of the 111 surveys completed, 82 (73.9%) re- spondents included one or more reasons for choosing to vaccinate or not to vaccinate children (Table 3). A trend (p = .08) was noted for a higher response rate among parents choosing not to vaccinate (86.4%) com- pared with the response rates of parents with children who were partially immunized (63.9%) or fully immunized (70.5%).
Among the 73.9% who listed multiple reasons, three primary reasons were identified for not vaccinating a child. These three reasons were as follows: parental beliefs of inadequate research on the effects of the vaccine on the child (48.6%), concerns related to ingredients in the vac- cine (14.3%), and adverse health reasons (11.4%). The parents of PV children cited three primary reasons for their decision. These reasons are a desire to use an al- ternative schedule for vaccinations (34.8%); concerns re- lated to possible reactions, side effects, or immune sys- tem response (30.4%); and belief of inadequate research (21.7%). The top three reasons cited by FV parents are belief of inadequate research (25%), adherence to guide- lines (16.6%), and advice of their healthcare provider or travel plans (12.5%). In regards to the finding re- search as a reason cited in favor of or opposed to vacci- nation, it is a primary underlying justification in all three groups.
Discussion
The current trend for many parents, supported by some healthcare providers, is to alter the vaccination schedule or delay vaccinations all together. One of the commonly given reasons is concerns of altered immune function in the child against all versions of childhood illnesses. This is at complete odds with the Healthy People 2020 goal of 80% vaccine coverage in the United States. Most studies to date have shown improved health outcomes in chil- dren who are vaccinated against vaccine-preventable ill- nesses and no alteration in immune function (IOM, 2002). Deficits in the evaluation of the nonvaccine-preventable illnesses are present in the current literature. Some re- cent studies have started to look at the correlation be- tween nonspecific infections, allergies, and eczema and vaccines (Kiraly et al., 2016; Schmitz et al., 2011). These studies lack a third comparison group that this study includes.
This study’s objective was to begin to understand the prevalence of childhood illnesses between the three vacci- nation groups. The hypothesis was that there are no differ- ences between FV, PV, and NV groups in the frequency of
childhood illnesses. This was not supported. We found dif- ferences between childhood illnesses and vaccination sta- tus.
This study examined children between 12 months and 7 years old accompanied by a parental survey on the child’s vaccine status, age, reason for choice for vaccine status, daycare or school attendance, other children in the home, and common childhood illnesses.
There was a high response rate of 97.6% with 81 parents filling out surveys for 111 children. The survey excluded children younger than 12 months or older than 7 years at the time of data collection. Only two parents declined to participate. This rate allows the data to be highly represen- tational of the population surveyed.
Current literature suggests that being FV, including the PCV-13 vaccine, correlates with decreased pediatric ear in- fections (Marom et al., 2014). Our study noted a statisti- cally significant increase in the occurrence of ear infections between the FV group and the other two groups com- bined. This was an unanticipated finding. More research is needed to determine if this finding should be attributed to age differences, the sample size used in this study, chance, or other possible causes.
A statistical association in the prevalence of viral illnesses between groups was found. Children in the NV group were more likely to have the flu (p = .05) and to expe- rience colds (p = .02) compared to the PV and FV group. These statistical differences may be related to a smaller sample size and that some children were members of the same family. It is entirely possible for one child to be pass- ing on an infection or illness to another in their household.
The findings of this study are consistent with previous studies in regards to the reasons parents make decisions about vaccinating their child. The most important rea- sons are concerns about safety, side effects, trust in pre- vious studies, and literature (Benin, Wisler-Scher, Colson, Shapiro, & Holmboe, 2006; Byström et al., 2014; Parrella, Gold, Marshall, Braunack-Mayer, & Baghurst, 2013; Sid- diqui et al., 2013; Yaqub et al., 2014). Adherence to guide- lines and advice from healthcare providers are often listed as significantly relevant (Connors et al., 2012) and were the reasons most often listed as influencing parental choice in the FV group. The results in this study agree with previ- ous studies which cite that older and well-educated par- ents make alternative choices for vaccines (Gust et al., 2008; Salmon et al., 2015). Although this study did not evaluate the age or education level of parents, all three groups consistently stated the desire for research on vac- cines and health outcomes, from unbiased sources as their reason for making vaccine choices. Other studies show that because older and educated parents are reviewing healthcare data and information before they make a de- cision regarding vaccination, between 10% and 15% of
421
Childhood vaccine status M. M. Anderson & C. Arvidson
parents are not trusting the available literature and are subsequently making decisions to alter the recommended schedule or to not vaccinate (Byström et al., 2014; Glanz, Kraus, & Daley, 2015).
A German study by Schmitz et al. (2011) utilized an FV group and an NV group. Their FV group included one or more vaccines given compared to our FV group which was inclusive of all age appropriate vaccines. We utilized a PV group to fill in the gap between our FV and NV group. Schmitz et al. utilized a larger age range from 1 to 17 years of age versus our 1 to 7 years. With their larger age range and study size they did not report the prevalence of aller- gies or infections related to vaccine status. Our study had a narrower age range and smaller subject size which could account for the statistical differences found.
When comparing the study findings to allergy and eczema components our population size was not large enough to see if there was a similar correlation such as that discovered by Kiraly et al. (2016). For some of the comparisons, such as eczema, the group number was not large enough to determine a p-value.
Limitations
There are potential limitations to our study. The first lim- itation is recall bias. The findings may be influenced by both recall and response bias of the parents which is a threat to validity. A chart review was done to evaluate for this and the findings were comparable. Parents can have difficulty in remembering the occurrence of illness and in some settings can confuse it with a different illness. Highly correlated illnesses are an additional potential limitation. The illnesses we tracked did correlate highly with each other, such as flu, vomiting, and diarrhea. These illnesses often are known to occur at one time and may be listed as different illnesses by one parent or the same illness by another.
A small sample size and population might not be fully representative of the general population. Further, a small study has a reduced chance of detecting a true effect. North Idaho is associated with the Western region which has tra- ditionally been known to have lower rates of vaccination secondary to philosophical beliefs in comparison to other U.S. geographical regions (Gust et al., 2008). Philosophi- cal beliefs, as a reason for vaccine choice, were no higher in the NV group than the others in our study, although sample size may have played a role in this effect. The small sample size along with the confounding variable of age dif- ference in the three groups cannot be discounted. The FV group is slightly more than 1 year older than the PV group and has thus had more opportunity to develop illnesses such as ear infections, which tend to diminish as a child ages.
Strengths and implications
The primary strengths of this study are the large overall response rate, the ability to represent three different vac- cine groups, the good representation of the data and the practice it was obtained from, and the validity of the most frequently reported illnesses.
The implications for NP practice based on this study and its findings relate directly to further research, educa- tion, support, and trust building. Further research with a larger sample size that would be more representative of the population would potentially help validate these findings and perhaps show further statistical differences among the other listed illnesses for which the sample size in this study was too small to evaluate. A longitudinal study on a larger number of children over 10 years would also shed light on these findings. Either way the information is important. Looking at the concerns vaccine-hesitant parents give from this viewpoint directly addresses the questions they typi- cally bring into an office visit. Although there were some statistical differences in common childhood illness occur- rence, these findings need to be weighed against the risk of vaccine-preventable illnesses when making an alterna- tive vaccine choice. NPs can utilize this information to help educate their patients’ parents in their practice who refer- ence concerns about less-immune response to nonvaccine- preventable illnesses. They are better able to guide them on the true risks versus benefits of their choice. Being able to share this information and provide further support and guidance in their decision-making process allows for con- tinued collaborative care, trust building, and better overall health outcomes.
Conclusion
Informing parents of the incidence of common child- hood illness between the vaccinating and nonvaccinating groups allows them to make vaccine and care decisions for their children from a position of strength and knowledge. This is a trust-building process that the NP is perfectly sit- uated to accomplish. If handled correctly, this will result in the best health outcomes for all involved, including a greater chance of obtaining the 80% vaccination Healthy People 2020 goal previously set.
Acknowledgments
The authors thank the following for their helpful advice and facilitation of the survey: Dr. Ana Schaper, PhD, RN, Adjunct Faculty, Idaho State University; Dr. Anne Church, DNP,MSN/PNP, North End Children’s Health Clinic, Boise, Idaho; and Susan Strobel, MPH, BA, RN-PHN Teaching Scholar Fellow, University of Colorado, Denver.
422
M. M. Anderson & C. Arvidson Childhood vaccine status
References
Alter, S. J., Vidwan, N. K., Sobande, P. O., Omoloja, A., & Bennett, J. S. (2011).
Common childhood bacterial infections. Current Problems in Pediatric and
Adolescent Health Care, 41, 256–283. Retrieved from http://doi.org/10.1016/
j.cppeds.2011.06.001
Andre, F. E., Booy, R., Bock, H. L., Clemens, J., Datta, S. K., John, T. J., . . .
Schmitt, H. J. (2008). Vaccination greatly reduces disease, disability, death
and inequity worldwide. Bulletin of the World Health Organization, 86(2),
81–160. Retrieved from http://www.who.int/bulletin/volumes/86/2/07-
040089/en/
Angoulvant, F., Jumel, S., Prot-Labarthe, S., Bellettre, X., Kahil, M., Smail,
A., . . . Alberti, C. (2013). Multiple health care visits related to a pediatric
emergency visit for young children with common illnesses. European Journal
of Pediatrics, 172(6), 797–802. Retrieved from http://doi.org/10.1007/s00431-
013-1968-9
Bakhache, P., Rodrigo, C., Davie, S., Ahuja, A., Sudovar, B., Crudup, T., & Rose,
M. (2013). Health care providers’ and parents’ attitudes toward
administration of new infant vaccines—A multinational survey. European
Journal of Pediatrics, 172(4), 485–492. Retrieved from
http://doi.org/10.1007/s00431-012-1904-4
Benin, A. L. Wisler-Scher, D. J., Colson, E., Shapiro, E. D., & Holmboe, E. S.
(2006). Qualitative analysis of mothers’ decision-making about vaccines for
infants: The importance of trust. Pediatrics, 117(5), 1532–1541. Retrieved
from http://doi.org/10.1542/peds.2005-1728
Bryant, P. A., & Lester, C. M. (2014). Acute childhood exanthems. Medicine,
42(1), 52–56. Retrieved from http://doi.org/10.1016/j.mpmed.2013.10.002
Byström, E., Lindstrand, A., Likhite, N., Butler, R., & Emmelin, M. (2014).
Parental attitudes and decision-making regarding MMR vaccination in an
anthroposophic community in Sweden—A qualitative study. Vaccine, 32,
6752–6757. Retrieved from http://doi.org/10.1016/j.vaccine.2014.10.
011
Connors, J., Arushanyan, E., Bellanca, G., Racine, R., Hoeffler, A., Delgado, A.,
& Gibbons, S. (2012). A description of barriers and facilitators to childhood
vaccinations in the military health system. Journal of the American Academy of
Nurse Practitioners, 24(12), 716–725. Retrieved from http://doi.org/10.1111/
j.1745-7599.2012.00780.x
Dunn, A. C., Black, C. L., Arnold, J., Brodine, S., Waalen, J., & Binkin, N.
(2015). Childhood vaccination coverage rates among military dependents in
the United States. Pediatrics, 135(5), e1–e9. Retrieved from
http://doi.org/10.1542/peds.2014-2101
Epling, J. W., Savoy, M. L., Temte, J. L., Schoof, B. K., & Campos-Outcalt, D.
(2014). When vaccine misconceptions jeopardize public health. Journal of
Family Practice, 63(12), E1–E7.
Fernbach, A. (2011). Parental rights and decision making regarding
vaccinations: Ethical dilemmas for the primary care provider. Journal of the
American Academy of Nurse Practitioners, 23(7), 336–345. Retrieved from
http://doi.org/10.1111/j.1745-7599.2011.00627.x
Glanz, J. M., Newcomer, S. R., Narwaney, K. J., Hambidge, S. J., Daley, M. F.,
Wagner, N. M., . . . Weintraub, E. S. (2013). A population-based cohort study
of undervaccination in 8 managed care organizations across the United
States. Journal of the American Medical Association Pediatrics, 167(3), 274–281.
Retrieved from http://doi.org/10.1001/jamapediatrics.2013.502
Glanz, J. M., Kraus, C. R., & Daley, M. F. (2015). Addressing parental vaccine
concerns: Engagement, balance, and timing. Public Library of Science Biology,
13(8), e1002227–e1002227. Retrieved from
http://doi.org/10.1371/journal.pbio.1002227
Gust, D. A., Darling, N., Kennedy, A., & Schwartz, B. (2008). Parents with
doubts about vaccines: Which vaccines and reasons why. Pediatrics, 122(4),
718–725. Retrieved from http://doi.org/10.1542/peds.2007-0538
Institute of Medicine (IOM). (2002). In K. R. Stratton, C. B. Wilson, & M. C.
McCormick (Eds.), Immunization safety review: Multiple immunizations and
immune dysfunction. (pp. 1–20). Washington, DC: National Academy Press,
2002.
Kiraly, N., Koplin, J. J., Crawford, N. W., Bannister, S., Flanagan, K. L., Holt, P.
G., . . . Allen, K. J. (2016). Timing of routine infant vaccinations and risk of
food allergy and eczema at one year of age. Allergy, 71, 541–549. Retrieved
from http://doi.org/10.1111/all.12830
Marom, T., Tan, A., Wilkinson, G. S., Pierson, K. S., Freeman, J. L., &
Chonmaitree, T. (2014). Trends in otitis media-related health care use in the
United States, 2001-2011. Journal of the American Medical Association Pediatrics,
168(1), 68–75. Retrieved from http://doi:10.1001/jamapediatrics.2013.3924
Martin, M., & Badalyan, V. (2012). Vaccination practices among physicians and
their children. Open Journal of Pediatrics, 02(03), 228–235. Retrieved from
http://doi.org/10.4236/ojped.2012.23036
Office of Disease Prevention and Health Promotion (ODPHP). (2015).
HealthyPeople.gov: Immunization and infectious diseases. Retrieved from
https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-
and-infectious-diseases
Offit, P. A., & Moser, C. A. (2009). The problem with Dr. Bob’s alternative
vaccine schedule. Pediatrics, 123(1), e164–e169. Retrieved from
http://doi.org/10.1542/peds.2008-2189
Parrella, A., Gold, M., Marshall, H., Braunack-Mayer, A., & Baghurst, P. (2013).
Parental perspectives of vaccine safety and experience of adverse events
following immunisation. Vaccine, 31(16), 2067–2074. Retrieved from
http://doi.org/10.1016/j.vaccine.2013.02.011
Salmon, D. A., Dudley, M. Z., Glanz, J. M., & Omer, S. B. (2015). Vaccine
hesitancy: Causes, consequences, and a call to action. American Journal of
Preventive Medicine, 49(6 Suppl. 4), S391–S398. Retrieved from http://doi.org/
10.1016/j.amepre.2015.06.009
Schmitz, R., Poethko-Müller, C., Reiter, S., Schlaud, M., & Twisselmann, B.
(2011). Vaccination status and health in children and adolescents. Deutsches
Aerzteblatt International, 108(7), 99–104 6p. Retrieved from http://doi.org/10.
3238/arztebl.2011.0099
Scott, J. A. G., & English, M. (2008). What are the implications for childhood
pneumonia of successfully introducing hib and pneumococcal vaccines in
developing countries? Public Library of Science Medicine, 5(4), e86. Retrieved
from http://doi.org/10.1371/journal.pmed.0050086
Siddiqui, M., Salmon, D. A., & Omer, S. B. (2013). Epidemiology of vaccine
hesitancy in the United States. Human Vaccines & Immunotherapeutics, 9(12),
2643–2648. Retrieved from http://doi.org/10.4161/hv.27243
World Health Organization (WHO). (2009). Immunization, vaccines and biologicals.
Retrieved from http://www.who.int/immunization/givs/goals/en/
Yaqub, O., Castle-Clarke, S., Sevdalis, N., & Chataway, J. (2014). Attitudes to
vaccination: A critical review. Social Science & Medicine, 112, 1–11. Retrieved
from http://doi.org/10.1016/j.socscimed.2014.04.018
423
The post Childhood vaccine status and correlation with common nonvaccine-preventable illnesses Michelle M. Anderson, DNP, FNP (Family Nurse Practitioner)1 & Cathy Arvidson, PhD, FNP, RN, FAANP (Associate Professor)2 appeared first on Infinite Essays.
[ad_2]
Source link